Every year approximately 12.9 million babies—roughly 10 percent of all newborns around the world—are born too early, which is to say, before 37 weeks in utero. Despite a heroic, costly, and decades-long effort by doctors and scientists to understand and prevent preterm birth, that number has climbed steadily for the past three decades. In the U.S. alone, premature births are up 40 percent since 1980. Meanwhile, as modern medicine helps more and more of those babies survive, doctors and scientists have found themselves confronted with a new dilemma: how to prevent the string of neurological problems and developmental disabilities that plague many premature babies as they grow into children and adults.
Some of the factors behind the rise in preterm births are obvious: more women having children later in life (the risk of delivering prematurely increases as women get older), more families using in vitro fertilization (with its tendency toward multiple births), and more doctors opting for Caesarean sections at the first signs of fetal distress. But even among women who do none of these things, preterm births are still increasingly common. The fluid-filled membrane that surrounds the uterus ruptures decidedly ahead of schedule, sending mother into labor before baby is fully developed. Doctors still have no idea why this happens or how to prevent it. "Preterm birth is a huge, thriving area of research," says Amy McKenney, a perinatal pathologist at Stanford University Medical Center. "But for all of it, we haven't made much of a dent."
A $75 million educational campaign by the March of Dimes has managed to reduce incidence by a smidgen, from 12.8 percent in 2006 to 12.3 percent in 2008, mostly by persuading more pregnant women to quit smoking and more doctors to avoid elective C-sections in all but the direst cases.
But other efforts have failed spectacularly. "The most common interventions recommended to prevent or treat preterm labor have proved to be of little or no benefit," says Louis Muglia, a neonatologist at Vanderbilt University. For example, doctors learned in 2000 that certain bacterial infections increase a mother's chances of delivering early. But treating those infections with antibiotics does not reduce the risk of preterm delivery or improve the baby's prognosis. Likewise, women whose cervixes have shortened to less than 25mm in length by their second trimester are three times as likely to deliver early, according to studies done in 2001. But placing a cerclage, or stitch, in the cervix to help prevent further shortening has proved to be of almost no value. And while several clues point to a genetic component—preterm births tend to run in families and are higher in certain ethnic populations—the hunt for offending genes has been inconclusive at best.
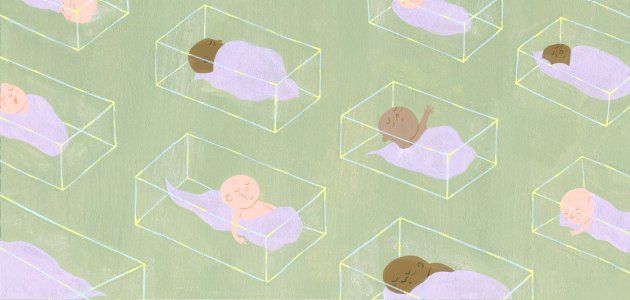
Where we have improved is in keeping preemies alive. As recently as 1940, babies who were born too early or too small were often listed as stillborn and left for dead. Today we devote entire hospital wings—not to mention $26 billion in annual health-care costs—to keeping the frailest of newborns alive. Like giant mechanical wombs, neonatal intensive-care units employ a vast array of machinery to protect preterm babies from the outside world: incubators isolate them from pathogens while a host of machines and medications regulates body temperature and keeps tiny lungs working until baby is strong enough to do those things on her own. The result: 80 to 98 percent of preemies born in the U.S. now survive.
But so far, not even the best hospital in the world can fully substitute for a mother's womb. Preemies who survive the neonatal intensive-care unit frequently go on to experience a range of developmental disabilities as they grow. Some suffer from behavioral problems like attention-deficit/hyperactivity disorder, others develop more serious conditions, including mental retardation, cerebral palsy, and, according to two recent studies, autism. And unlike lung or heart problems, which are immediately apparent, neurological impairment can take years to show up. "We are delivering more and more babies preterm, and we are saving more and more of them," says Anna Penn, a neonatologist at Packard Children's Hospital in California. "But neurological outcomes are not improving in tandem." To change this, scientists will have to figure out what forces guide fetal brain development in the first place. Penn and her colleagues are betting on the placenta, a thick layer of cells that envelops part of the fetus.
Ancient civilizations, at least, were keenly aware of the placenta's significance, even if they lacked the scientific tools to probe its depths. Convinced of its mythical powers, the Egyptians built a cult around royal afterbirth—preserving and protecting the pharaoh's placenta while the king was alive, and burying it with him when he died. The latter custom—placenta burial—is still practiced by dozens of religious groups around the world today.
But as far as organs go, the placenta has ranked pretty far down on the totem pole for most of the modern medical era. Doctors recognized its ability to protect the fetus from a range of potential assaults and to usher a few basic chemicals, like oxygen and carbon dioxide, across the mother-fetus divide, but never suspected it was an actual organ capable of interacting with both mother and fetus. In fact, most doctors still toss the blubbery disc-shaped mass into an incinerator-bound bucket almost as soon as the mother expels it from the womb.
It turns out that the placenta is an organ, and a complicated one at that. Genetically all fetus but intricately bound to the mother's blood vessels, it facilitates a constant chemical dialogue between expecting mother and unborn child. It's this dialogue—nutrients, gasses, and hundreds of placenta-made hormones streaming back and forth—that transforms a fetus into a sufficiently developed infant.
A steady beat of emerging research suggests that crucial instructions for later neurodevelopment may also be included in that conversation. By manufacturing a vast array of chemicals and deploying them to the fetus, where they cross the blood-brain barrier, the placenta sets in motion a cascade of chemical events whose effects won't be fully realized for years to come.
Penn and her colleagues reason that cutting the conversation short leaves the developing brain in the lurch. "Without the placental signposts, development is hobbled," she says. "If we can figure out exactly what directions have been lost, we can chart an identical map and help keep development on course."
Using a small army of genetically engineered mice, Penn's team is turning off one hormone gene at a time in the hopes of determining which of them has the biggest impact on neural development. On top of that, they are collecting blood and spinal fluid from human babies—both premature and full term—so that they can compare hormone profiles between groups.
So far, two particular chemicals have emerged as potential culprits. Both progesterone, which helps nerve cells to grow, and oxytocin, which protects fetal neurons from becoming over-excited and dying, appear to reach peak concentrations late in pregnancy. That means a baby who's born even a few weeks prematurely could be missing out on a crucial dose.
Oxytocin—sometimes called the cuddling hormone for its role in emotional attachment and maternal behavior—has also been implicated in autism. In young children, low concentrations of the hormone have been linked to social and behavioral difficulties, and signaling pathways for oxytocin have been shown to be impaired in autistic children.
That's not the only factor placing autism and preterm labor in the same orbit; both autism and the worst developmental effects of premature birth are more than twice as prevalent in males. And in a study published last year, children who were born significantly prematurely (before 27 weeks in utero) were twice as likely to develop autism. Penn and her Stanford colleagues are comparing oxytocin levels between 2-year-olds with autism and 2-year-olds without the disorder who were all born prematurely. "We want to see if the two groups have similar hormone profiles," says Penn. "It could mean that both are caused by some unique placental malfunction."
Once doctors understand which hormones are essential to fetal brain development, Penn hopes they will be able to measure the level of those hormones in the premature baby's blood and replace what's missing quickly enough to stave off neurological disaster.
Before they get there, many more human placentas will have to be studied. Penn's team is vying to build a large placenta repository, like the ones cancer biologists use to share and study tumor samples. Until that happens, some of the most valuable clues to brain development will continue to be tossed into the trash.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
To read how Newsweek uses AI as a newsroom tool, Click here.