The head of the World Health Organization has called the world’s second worst Ebola outbreak a “global wake-up call” to the escalating risk of disease outbreaks spreading from conflict areas neglected by the international community.
Only when there was “fear and panic” in the headlines did the international community put money into responding, said Dr Tedros Adhanom Ghebreyesus. The real issue was a lack of day-to-day funding for preparedness to combat serious epidemics before they become regional or international threats, he said.
Speaking ahead of a new call for funding for the response to the Ebola outbreak, he added: “The problem is that [donors] refrain from paying until there is fear and panic. That has to change. We should not be funding by huge amounts when we panic, but should be funding to avoid panic.”
Invoking the spectre of Spanish influenza, which killed tens of millions in the aftermath of World War I, he added that international health systems in an increasingly globalised world were only as “strong as the weakest link”.
In an exclusive interview with the Guardian in Geneva, Tedros added that while he believed the outbreak in the Democratic Republic of the Congo could be controlled in the short term – given the right security conditions – the virus would inevitably return while political instability continued in North Kivu and Iruri, the provinces at the heart of the outbreak.
Quick GuideEbola in the Democratic Republic of the Congo
Show
How bad is the current outbreak?
With more than 2,577 confirmed cases and more than 1,803 confirmed deaths, the outbreak in the eastern DRC is the second largest in history. It has a 67% fatality rate and 11 months after it began, the case numbers are still escalating. It is disproportionately affecting women (55% of cases) and children (28%).
The WHO declared the outbreak an international public health emergency in July 2019. The same month saw the the first diagnosis of a case in Goma, a city of 2 million people, which is a transport hub on the border with Rwanda. In early August Rwanda announced that it was closing its border with DRC.
The WHO has long said that the national and regional risk levels are very high and containment of the spread to North Kivu and Ituri provinces was unlikely, unless a break in the fighting made it safe for health workers.
What is Ebola and how do you treat it?
Ebola hemorrhagic fever is caused by a virus that has a reservoir among forest animals, including monkeys and bats. It is spread through body fluids, which is why carers – mostly female relatives and nursing staff – are particularly at risk. It causes fever, aches and diarrhoea and attacks the immune system, causing blood clotting cells to malfunction so that victims bleed extensively and die if their immune system cannot fight off the viral infection.
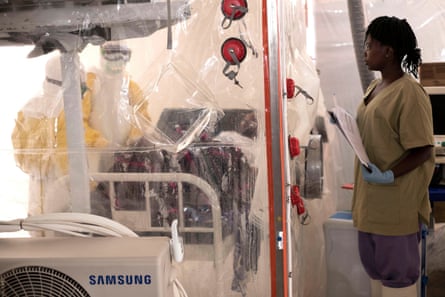
Drugs are still experimental. Patients are isolated and treated by nurses wearing full protective body suits and masks who try to boost their immune response. Friends and relatives are quarantined for 21 days. Prevention measures include washing hands at every opportunity and safe burial practices, with no touching or washing of the body, as is traditional in some cultures.
How does this compare with other outbreaks?
The 2013 and 2016 outbreak in Sierra Leone, Liberia and Guinea spread for months through forest regions in west Africa where Ebola was unknown before the emergency was recognised. It escalated when it emerged in towns and cities, with 28,600 cases and 11,300 deaths.
DRC successfully stamped out nine previous Ebola outbreaks in rural areas within a matter of a few months. Aid agencies, infectious disease experts and the WHO say it will be very hard to bring this outbreak under control, even though they have had vaccines and experimental drugs from the outset.
What are the contributing factors to this outbreak?
There is almost no functioning state in much of eastern DRC. There is an almost total lack of basic services such as power, education, roads, healthcare, and the authority of the government only extends to the edges of urban areas.
Police are corrupt, predatory and violent. In rural zones, militia and armed bands provide security and employment opportunities but also steal, rape and kill at will. It is one of the most hostile environments faced by aid and health workers anywhere in the world.
Mistrust of officials and foreigners is harming efforts to tackle the disease and conspiracy theories are rampant. Some believe the outbreak is fake news spread by rapacious NGOs and the UN to justify their presence in the country and allow the extraction of valuable mineral resources.
Tedros also reiterated his resistance to declaring the current outbreak a public health emergency of international concern (PHEIC). This is despite calls from the British international development secretary, Rory Stewart, during a visit to the city of Butembo, the current epicentre of the outbreak.
“I know we can finish this Ebola outbreak,” said Tedros, former foreign minister of Ethiopia, who became director general of the UN global health organisation in 2017. “But at the same time it can come back because all the [political and security] conditions remain the same.
“There are some people who say we need to declare the outbreak as an [emergency] to mobilise resources. That’s really wrong. Resources should be available to prevent needing to declare a PHEIC. Preparedness is the solution, not firefighting.”

WHO officials also questioned Stewart’s assertion in the Guardian that more cash was needed to pay for ring vaccination. They said that at present there was a sufficient supply for the current models of the epidemic, although in the longer term, this would depend on the evolution of the outbreak.
The outbreak is designated a “category three emergency”, the WHO’s highest level before a declaration of PHEIC. Three cases crossed the border briefly into Uganda last month.
Tedros warned, however, that far from helping with the response to the outbreak, designating it as a PHEIC could actually complicate the response of health teams on the ground. It could see borders closed and increase economic hardship for an already highly marginalised and angry population that relies on cross-border trade and has already attacked health teams.
Briefing a meeting of science journalists on Friday, ahead of Stewart’s intervention, Tedros reiterated his objections.
“PHEIC only shows there is a very high risk of international spread, which is not the case based on the criteria. But if you take whether Ebola is an emergency in DRC or not, it is – it’s actually the highest level of emergency.”
Although outbreaks of the disease in the neighbouring town of Beni and surrounding areas were largely brought under control last year, the outbreak in Butembo has proved hugely complicated, with violent attacks on health officials and treatment centres.
The WHO has attracted criticism for its response to the DRC outbreak, not least over the issue of whether to declare it a global health emergency, a move critics say could prompt more donor countries to offer funds and other resources.
“I’m not saying we cannot learn lessons and there was no shortfall,” Tedros told the Guardian, adding that the organisation would conduct a proper assessment of the current response.

“But we have never had conditions like this in other places where we have had Ebola.”
As an example of the political issues facing the response to the Ebola crisis, Tedros cited the DRC government’s decision to cancel voting in national elections in the Ebola-affected areas, as the outbreak moved to the city of Butembo last autumn.
“When we heard about the decision to cancel the elections we said: ‘Don’t do that. It’s dangerous,’” he said, adding that he had personally appealed to ministers in the DRC as well as the African Union to reverse the decision.
“That was a game-changer, to be honest,” he added. “An opportunity was missed and the community was angered and started attacking the responders.”
Like other senior health officials involved in the response on the ground, Tedros blamed highly complex political and security issues for resurgences in the outbreak.
“The political problems [in DRC] have broken the whole system – social, economic and so on. And to be honest when I talk to the community it is embarrassing for me, because they say, ‘You are only interested in Ebola because you do not want it in your own countries and you are trying to protect yourselves while mothers and children are dying here.’
“The root cause of the problem is lack of peace, the lack of a political solution. The incidence of Ebola, malaria and cholera is the symptom.
“It’s not about Ebola only. What concerns me is the lacking of understanding about how to make our world safe,” he said, citing the risk of an airborne pandemic.
“We’re not investing in preparedness to detect outbreaks quickly. We are investing after the problem comes and knocks on our door when it’s too late. So how can we move on from that mindset? We have to be as strong as the weakest link and we need to invest in strengthening the systems of the weakest link.
“We think that we are very far from the problem but in a globalised world even if it is only happening in one country it can be exported – so there is a risk, even as we speak, of spread. We should support the Congolese but also help ourselves.”